Children in hospital: a guide for family and carers by Richard Lansdown
Oxford University Press (Oxford Medical Press) (1996) ISBN: 0-19-262357-5
“Matching the intervention to the child”…
Although the book is over 20 years old, families, healthcare professionals, early childhood educators and students will find a useful overview supporting children in hospital and healthcare. Researchers continue to read this book today.
Child rights
Have we come to expect child-friendly services? Lansdown writes about early hospitals and emotional aspects such as separation and the battle of early visitors, this gives a significant background. Development of child rights in hospital, saw the emergence of advocacy organisations and the Charter for children in hospitals, NAWCH 1984.
In Australia, AWCH promoted child rights and better healthcare with Health care policy relating to children and their families published 1974, revised 1999 and Charter on the rights of children and young people in healthcare services, 2010. Understanding child rights in healthcare is essential. An 11 year old girl on a children’s ward in the UK asks “aren’t we kids supposed to have a bill of rights when we are in hospital?”, Children’s hospital charter revisited.
Fear and coping
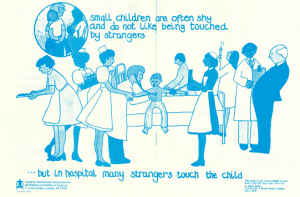
Children and families going to hospital or healthcare appointments may be fearful, Lansdown approaches the topic from a child’s perspective without being simplistic. You will find practical information about children’s understanding of health, illness and treatment. Play in hospital and play specialists (also known as child life therapists or specialists) guide children towards meeting their emotional needs.
Pain
The chapter on pain gives an understanding of its impact on children. Information and support are based on the child’s developmental stage and what works for them. Supportive strategies for children facing painful procedures include active distraction. This may involve reading books, toys, songs, stories, video games, mobile apps and new technologies such as video goggles. Other supportive strategies are participation, desensitization and modelling, watching a film that shows other children and mastery coping or coping models (initial anxiety then coping). Being noisy (counting out loud), guided imagery, relaxation and breathing techniques are some more options to consider.
A combination of distraction strategies might be used such as bubble blowing and guided imagery. For example, a child is asked to visualize the colour of the pain and places it on a bubble as though it was an imaginary cloud floating away. As the pain moves off, the bubble changes to the child’s favourite colour, blowing away pain and fear (p 116).
Talking with children
Summaries of pain assessment tools show how children rate their pain. Why ask children about pain? Adults usually explain how important a procedure is but there could be a gap in the child’s thinking. For example, a finger prick/injection to take blood may leave some children wanting information about why it is being done and what will happen next with the blood.
More information
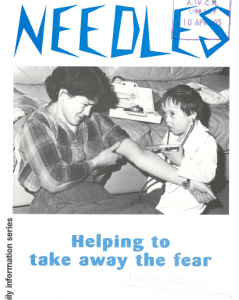
For more information about supporting children through medical procedures, see Needles and Needle-Related Medical Procedures links.
AWCH also holds a copy of Needles: helping to take away the fear, a booklet for parents based on information provided by Dr Richard Lansdown produced by Action for Sick Children, 1994.